Conditions >>
Imagine taking a step and feeling as if a stone is lodged deep in your heel. While that kind of pain can come from several causes, one possible finding is a heel spur. This refers to a small bony outgrowth, called a calcaneal spur, that develops on the heel bone. Despite the name, the spur itself is rarely the source of pain. More often, the discomfort comes from nearby tissues such as the plantar fascia or the Achilles tendon.
To understand why heel spurs form, it helps to look at how this part of the foot works as a weight-bearing structure. With every step, pressure travels through the heel, especially at the points where tendons and ligaments attach. When these areas are placed under repeated strain due to long hours on hard floors, frequent running, or footwear that lacks support, the body responds by depositing calcium. Over time, these deposits can harden into a spur. Because this process is gradual and often silent, many people only learn they have a spur when it shows up on an X-ray.
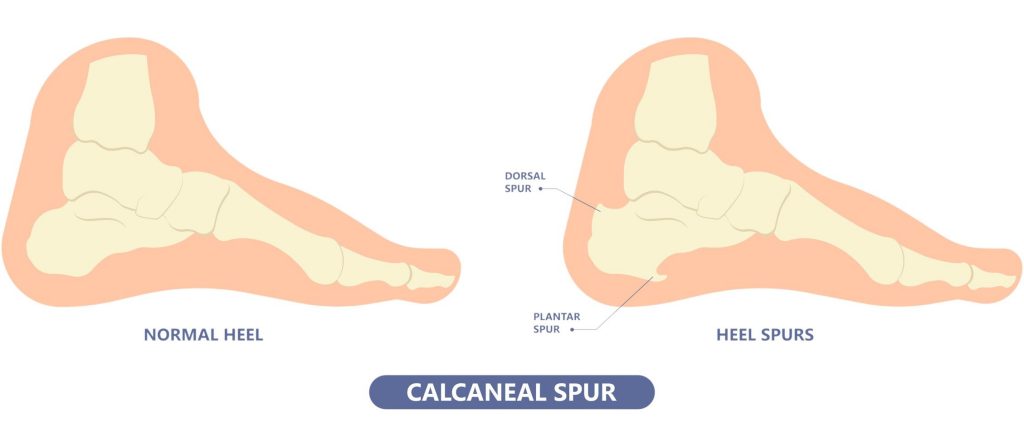
The position of the spur also adds context. Plantar spurs form on the underside of the heel, while posterior spurs develop at the back where the Achilles tendon connects. Since heel pain can arise from many different conditions, the presence of a spur does not always explain the pain. To see when it becomes significant, it helps to look more closely at the symptoms linked to heel spurs.
Although heel spurs can look dramatic on an X-ray, they are usually silent. More often, the soreness you feel comes from the tissues around the spur rather than the bony growth itself. Consequently, many people who think they have spur pain are actually dealing with plantar fasciitis or, less commonly, Achilles tendonitis.
When a heel spur does cause trouble, it’s typically because it rubs or presses on the attached tissue. This might produce heel pain that can be sharp, dull, or occasionally throbbing. In addition, swelling and tenderness can appear at the base or back of the heel, and the discomfort often intensifies when walking barefoot or exercising in shoes that lack support.
At times, you might notice a small bump beneath or behind the heel. If nearby nerves are irritated, the sensations can broaden beyond pain to include tingling, numbness, or a burning feeling. Since these features overlap with other causes of heel pain, a careful assessment by a podiatrist helps determine whether the spur is truly responsible and sets the stage for diagnosis and pain management.

Heel spurs develop as a reaction to ongoing stress at the bottom of the heel. When the plantar fascia repeatedly pulls on its attachment to the heel bone during movement, small areas of strain begin to form. In trying to repair this micro-trauma, the body deposits extra bone at the site. Over time, these deposits can harden into a spur. Because anything that increases pulling forces on the heel can add to this process, it is helpful to look at what drives spur formation and who carries higher baseline risk.
With the causes of heel spurs established, the next step is management and prevention. Here the aim is to ease strain on the heel and support recovery. The following section looks at practical ways to achieve this.
The heel works like a shock absorber with every step, absorbing and transferring force through the foot. Because of this constant loading, problems often arise in the tissues that anchor to the heel bone rather than from the spur itself. When a heel spur is present, the focus of management is therefore on reducing strain in these tissues instead of removing the bone. From there, care begins with calming irritation and gradually progresses to rebuilding strength and flexibility so the heel can handle daily load more comfortably.
The first step is to settle pain and give the heel better support:
Once symptoms ease, the next goal is to restore movement and improve resilience:
If discomfort or pain persists despite these steps, more targeted options should be considered:
Finally, prevention ensures progress is maintained. Replacing worn shoes before support is lost, wearing cushioned shoes on hard floors at home, and keeping the calves flexible and feet strong all help to reduce strain. Training should be built up gradually, with low-impact sessions included to share the load. By responding to heel pain early and maintaining these habits, the risk of recurrence is greatly reduced.

Hearing that you have a heel spur can feel alarming, especially if you picture a sharp bony spike causing every step to hurt. In reality, most spurs are painless, and the discomfort or pain often comes from the surrounding tissues rather than the spur itself. At Straits Podiatry we explain this clearly, so you understand what is really driving your symptoms and why procedures rarely target the bone directly.
From there our podiatrists assess your foot mechanics, footwear, daily activities and training load to identify the true source of stress on your heel. With these insights we craft a practical plan that reduces strain, restores comfort, and helps you move confidently again. If focused options such as ESWT are needed, they are added as part of a complete approach. Book a consultation today and take the next step toward clarity and pain relief.
Heel spurs form when repeated stress on the plantar fascia creates strain where it attaches to the heel bone, often due to running, prolonged standing, or wearing unsupportive shoes. Management focuses on easing pressure through supportive footwear, custom orthotics, stretching, and physical therapy, with advanced options such as ESWT considered if discomfort or pain persists.
Heel spurs are often found on X-rays taken for heel pain, though the spur itself may not be the source of discomfort. A podiatrist will review your symptoms, activity history, and foot mechanics to determine whether the pain is coming from the spur or from nearby tissues such as the plantar fascia.
A heel spur may feel like a hard bump or a sharp, pointy spot when touching the heel. Many people notice pain when walking, running, or even standing, often described as a jabbing sensation. The bone itself does not hurt, but the surrounding tissues can become irritated, which is what leads to discomfort during movement.
What does plantar fasciitis have to do with heel spurs?
Heel spurs often develop in people who have long-standing plantar fasciitis, as the repeated pulling of the inflamed plantar fascia can encourage calcium buildup on the heel bone. While a spur does not cause plantar fasciitis, the two conditions frequently appear together and might produce similar heel pain symptoms, which is why they are often discussed side by side.
Once a heel spur has developed, it does not shrink or disappear by itself. A podiatrist can assess whether the spur is contributing to pain or if the discomfort is coming from surrounding tissues such as the plantar fascia or Achilles tendon and then guide you on the best way to manage it.